Mental health religion: It’s a topic that often gets brushed under the rug, but it’s seriously important. We’re diving deep into how religious beliefs, practices, and communities impact mental health – both positively and negatively. Think about it: Does your faith help you cope with stress, or does it add to your anxieties? We’ll explore the complex interplay between spirituality and mental well-being, examining everything from prayer’s effects on the brain to the potential harms of religious trauma.
Get ready for a no-holds-barred look at this fascinating and often overlooked intersection.
This exploration will cover a wide range of perspectives, considering how different faiths approach mental illness, the role of religious leaders in providing support (or unintentionally causing harm), and the effectiveness of various religious coping mechanisms. We’ll also look at the cultural and societal factors that influence how people experience and address mental health within their religious context. Ultimately, our goal is to foster a more nuanced understanding of the relationship between faith and mental health, promoting open dialogue and informed decision-making.
Seeking Spiritual Support for Mental Health Challenges
For many, faith and spirituality play a significant role in navigating life’s challenges, including mental health struggles. The intersection of faith and mental wellness is complex, offering both potential benefits and limitations that deserve careful consideration. This section explores the ways in which religious communities and beliefs can contribute to mental health support, examining both successful interventions and the importance of understanding potential drawbacks.
The Role of Faith-Based Communities in Providing Mental Health Support
Faith-based communities often offer a crucial network of support for individuals facing mental health challenges. Congregations can provide a sense of belonging, shared values, and mutual understanding, fostering a supportive environment where individuals feel safe to share their struggles and receive empathy and encouragement. Pastors, priests, rabbis, and other religious leaders can offer spiritual guidance, pastoral counseling, and practical assistance, connecting individuals with resources and support networks within their community.
Many faith-based organizations also offer specific programs and initiatives focused on mental health, such as support groups, educational workshops, and referral services to professional mental health providers. The sense of community and shared faith can be particularly powerful in mitigating feelings of isolation and shame often associated with mental illness.
Examples of Effective Interventions Integrating Religious Beliefs and Mental Health Therapies
Several effective interventions successfully integrate religious beliefs and mental health therapies. One example is faith-based cognitive behavioral therapy (CBT), which adapts traditional CBT techniques to incorporate clients’ spiritual beliefs and values. This approach helps individuals identify and challenge negative thought patterns while drawing on their faith for strength and resilience. Another example is spiritual integration therapy, which explores the role of spirituality in a client’s life and how it can be leveraged to promote healing and well-being.
This approach might involve prayer, meditation, or other spiritual practices alongside traditional therapeutic techniques. For example, a therapist might work with a client to understand how their faith informs their coping mechanisms and help them develop healthier spiritual practices to manage stress and anxiety.
Experiences of Individuals Finding Solace and Healing Through Faith
Numerous individuals have shared their experiences of finding solace and healing through their faith during mental health struggles. Many testify to the power of prayer, meditation, and community support in providing comfort, hope, and a sense of connection during difficult times. For instance, a person struggling with depression might find comfort in attending church services, participating in a faith-based support group, or engaging in private prayer and reflection.
The shared experience of faith with others can create a sense of belonging and validation, reducing feelings of isolation and stigma. The belief in a higher power and the promise of divine support can also provide a sense of hope and purpose, even amidst suffering. These narratives highlight the profound impact that faith can have on mental well-being.
Potential Benefits and Limitations of Seeking Spiritual Guidance for Mental Health Concerns
It’s crucial to understand both the potential benefits and limitations of seeking spiritual guidance for mental health concerns.
- Benefits: Increased sense of hope and purpose, enhanced coping mechanisms, strong social support network, reduced feelings of isolation and stigma, access to faith-based resources and programs.
- Limitations: Potential for spiritual bypassing (avoiding emotional processing through spiritual practices), lack of professional mental health training among spiritual leaders, potential for judgment or stigma within some religious communities, conflicting advice between spiritual and secular approaches, reliance on faith as the sole treatment for severe mental illness.
The Intersection of Religious Doctrine and Mental Illness Stigma
The relationship between religious belief and mental illness is complex, often marked by both significant support and unfortunately, persistent stigma. While many faiths offer comfort, community, and a framework for understanding suffering, certain interpretations of religious doctrine can inadvertently contribute to negative attitudes towards mental health conditions. This intersection warrants careful examination to understand how religious beliefs can both help and hinder individuals seeking help for mental health challenges.Religious teachings can contribute to stigma in several ways.
For example, some interpretations emphasize willpower and personal responsibility, potentially leading to the belief that mental illness is a sign of personal weakness or a lack of faith. This can discourage individuals from seeking help, fearing judgment or exclusion from their religious community. Conversely, certain religious perspectives offer a framework for understanding suffering as a part of the human experience, emphasizing compassion and the importance of community support.
These approaches can foster a more accepting and supportive environment for individuals struggling with mental illness.
Religious Leaders’ Influence on Mental Health Acceptance
The attitudes and actions of religious leaders significantly impact how mental illness is perceived and addressed within their communities. When leaders openly discuss mental health, offer support to those struggling, and encourage seeking professional help, it creates a more accepting environment. Conversely, when leaders express disapproval or skepticism towards mental health treatment, or when silence surrounds the issue, it reinforces stigma and discourages individuals from seeking help.
The power of a religious leader’s voice to either alleviate or exacerbate stigma cannot be understated; their pronouncements shape the beliefs and behaviors of their followers. For example, a pastor who publicly shares his or her own experience with anxiety or depression can normalize mental health struggles and encourage others to seek help.
So, like, finding solace in religion for mental health is a totally valid path for some people. But, honestly, a solid routine also helps—check out this article on mental health exercise for some ideas. Regular physical activity can be a huge mood booster, which, you know, complements any spiritual practices you might have going on for a more holistic approach to mental well-being.
Challenges Faced by Individuals Seeking Mental Health Help Within Religious Communities
Individuals seeking mental health support within religious communities often face unique challenges. Some may fear judgment or exclusion from their community if they disclose their struggles. Others may encounter resistance from religious leaders or members who advocate for prayer or spiritual healing as the sole solution, potentially delaying or preventing access to necessary professional care. The conflict between faith-based approaches to healing and evidence-based mental health treatments can be particularly difficult for individuals to navigate.
This conflict can create a sense of isolation and exacerbate feelings of shame and guilt. For instance, a person struggling with depression might feel conflicted between seeking therapy, which is seen as helpful by their doctor, and the expectations of their church community to rely solely on prayer.
Religious Narratives and the Understanding of Mental Illness
Religious narratives and interpretations profoundly shape individuals’ understanding of mental illness. Some religious texts contain stories of individuals experiencing emotional distress or mental health challenges, offering a sense of validation and hope. However, the interpretation of these narratives can vary significantly. Some interpretations might emphasize the spiritual or demonic nature of mental illness, potentially leading to stigmatization and a reluctance to seek professional help.
Conversely, other interpretations may view mental illness as a form of suffering that requires compassion and support. The way these narratives are interpreted and conveyed within religious communities directly influences how individuals understand and cope with their mental health conditions. For instance, the biblical story of Job, while often cited as an example of suffering, can be interpreted in various ways, some potentially reinforcing the idea of mental illness as punishment or divine judgment.
Religious Coping Mechanisms and Their Effectiveness
Religious coping refers to the ways individuals utilize their faith and religious beliefs to manage stress, anxiety, and other mental health challenges. These strategies can be incredibly diverse, ranging from prayer and meditation to seeking pastoral support and engaging in religious rituals. Understanding the effectiveness and potential risks of these mechanisms is crucial for providing comprehensive mental health care.
Types of Religious Coping Strategies
Individuals employ a variety of religious coping strategies. Some actively seek spiritual guidance and meaning through prayer, Bible study, or attending religious services. Others find comfort in religious community and support networks. Some may focus on self-blame or questioning their faith in the face of adversity, while others may reinterpret their suffering as having spiritual significance. These strategies can be broadly categorized as positive, negative, or proactive.
Positive coping involves seeking spiritual support and finding meaning in faith. Negative coping involves self-blame, anger towards God, or spiritual disengagement. Proactive coping anticipates challenges and utilizes faith to prepare and prevent future problems.
Efficacy of Religious Coping Mechanisms
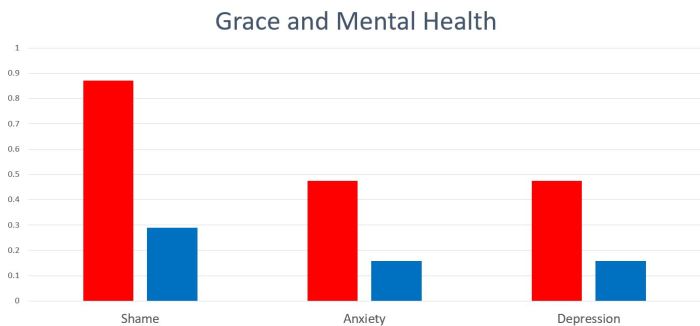
The effectiveness of religious coping varies significantly depending on the individual, their specific beliefs, and the nature of their mental health challenge. Studies have shown that positive religious coping, such as prayer and seeking spiritual support, can be associated with reduced stress, anxiety, and depression in some individuals. This is likely due to the sense of comfort, hope, and social support these strategies provide.
However, the impact isn’t uniform; for some, these strategies might be ineffective or even exacerbate existing issues. Negative religious coping, such as questioning one’s faith or feeling abandoned by God, is often linked to increased distress and poorer mental health outcomes. The effectiveness also depends on the individual’s interpretation of their religious beliefs and how they integrate them into their life.
Potential Risks of Maladaptive Religious Coping Strategies
While religious coping can be beneficial, maladaptive strategies can be detrimental. For example, relying excessively on prayer while neglecting necessary medical or psychological treatment can delay recovery. Similarly, self-blame and feelings of divine punishment can lead to increased guilt, shame, and depression. In some cases, individuals may withdraw from social support networks, isolating themselves and hindering their ability to cope effectively.
It’s also important to acknowledge that some religious beliefs and practices might conflict with evidence-based mental health treatments, leading to a reluctance to seek professional help.
Categorization of Religious Coping Mechanisms
| Coping Mechanism | Effectiveness | Potential Drawbacks | Example |
|---|---|---|---|
| Positive Religious Coping (e.g., prayer for strength, seeking pastoral support) | Generally effective in reducing stress and promoting well-being for many. | May delay seeking necessary professional help; potential for dependence. | Regular attendance at church and prayer for guidance during a difficult time. |
| Negative Religious Coping (e.g., self-blame, anger towards God) | Often ineffective; may exacerbate symptoms of anxiety and depression. | Increased guilt, shame, and feelings of isolation. | Believing a mental illness is divine punishment. |
| Proactive Religious Coping (e.g., spiritual preparation for challenges, faith-based problem-solving) | Can be effective in building resilience and coping skills. | Requires strong faith and may not be applicable to all situations. | Developing a spiritual plan for managing stress before a major life event. |
| Spiritual Disengagement (e.g., distancing from faith due to suffering) | Can be both helpful and harmful depending on individual circumstances. | Potential for increased feelings of isolation and loss of meaning; however, it might be a necessary step for some individuals. | Temporarily ceasing religious practices to process grief and disillusionment. |
The Role of Prayer and Meditation in Mental Well-being

Prayer and meditation, practices deeply rooted in many religious and spiritual traditions, are increasingly recognized for their potential to positively impact mental well-being. These practices, while often intertwined with faith, offer a range of physiological and psychological benefits that can be accessed regardless of religious affiliation. This section explores the evidence supporting their effectiveness in stress reduction, emotional regulation, and overall mental health.
Physiological and Psychological Effects of Prayer and Meditation, Mental health religion
Prayer and meditation elicit measurable changes in the body and mind. Physiologically, studies have shown that regular practice can lower blood pressure, heart rate, and cortisol levels (the stress hormone). This reduction in physiological stress markers contributes to a sense of calm and relaxation. Psychologically, these practices can cultivate self-awareness, improve focus and concentration, and enhance emotional regulation skills.
The ability to observe thoughts and feelings without judgment, a key component of mindfulness meditation, can help individuals manage negative emotions more effectively and prevent them from escalating into distress. This process reduces rumination and promotes a sense of acceptance.
Evidence-Based Research on Stress Reduction and Emotional Regulation
Numerous studies support the beneficial effects of prayer and meditation on stress reduction and emotional regulation. For instance, research published in theJournal of Consulting and Clinical Psychology* demonstrated that mindfulness-based stress reduction (MBSR) programs, incorporating meditation techniques, significantly reduced anxiety and depression symptoms in participants compared to control groups. Similarly, studies on the effects of prayer have shown a correlation between regular prayer and lower levels of perceived stress and improved mood.
While the mechanisms are not fully understood, it’s hypothesized that the act of prayer, whether it involves verbal communication or quiet contemplation, can activate the parasympathetic nervous system, responsible for the body’s “rest and digest” response, counteracting the effects of the sympathetic nervous system activated during stress.
Comparison of Prayer and Meditation with Other Mental Health Interventions
While not a replacement for professional mental health treatment, prayer and meditation have shown comparable effectiveness to some other interventions for specific conditions. Studies comparing meditation to cognitive behavioral therapy (CBT) for anxiety disorders have indicated that both can be effective, although CBT often involves a more structured approach to cognitive restructuring. The relative effectiveness of prayer and meditation compared to other interventions, such as medication, depends heavily on the individual, the specific condition being addressed, and the context of the intervention.
For example, prayer might be particularly helpful for individuals who find solace and comfort in their faith, while medication may be more appropriate for individuals experiencing severe symptoms requiring immediate and targeted pharmacological intervention.
Neural Pathways Activated During Prayer and Meditation
A visual representation of the neural pathways activated during prayer and meditation would depict increased activity in several key brain regions. Imagine a brain image with highlighted areas. The prefrontal cortex, responsible for executive functions like attention and emotional regulation, would show increased activity, represented by a brighter color. The amygdala, associated with fear and anxiety processing, would show decreased activity, depicted by a dimmer color.
The hippocampus, involved in memory and learning, and the insula, associated with self-awareness and interoception (awareness of bodily sensations), would also show increased activity, again indicated by brighter coloration. Connections between these regions would be visually emphasized, illustrating the interconnectedness of these brain areas during meditative states. The overall image would convey a shift from a state of heightened amygdala activity (associated with stress) towards increased activity in prefrontal cortical areas and other regions associated with self-regulation and emotional processing.
This visual representation would emphasize the neurobiological basis of the mental health benefits associated with prayer and meditation.
Religious Leaders’ Training in Mental Health Awareness: Mental Health Religion

Religious leaders often occupy positions of significant trust and influence within their communities, making them uniquely positioned to identify and support individuals struggling with mental health challenges. Equipping these leaders with the necessary knowledge and skills is crucial for fostering a more supportive and understanding environment within religious settings. Failure to do so can inadvertently perpetuate stigma and hinder individuals from seeking help.The benefits of comprehensive mental health training for religious leaders are multifaceted.
Improved training leads to more accurate identification of mental health issues, enabling earlier intervention and access to appropriate care. It also fosters empathy and understanding, reducing the stigma associated with mental illness within religious communities. Furthermore, trained religious leaders can effectively integrate faith-based approaches with professional mental health services, creating a holistic and supportive care system.
Successful Initiatives Integrating Mental Health Awareness into Religious Education
Several successful initiatives demonstrate the effectiveness of integrating mental health awareness into religious education. One example is the collaboration between seminaries and mental health organizations, offering specialized courses on pastoral care and mental health. These courses typically cover topics such as recognizing the signs and symptoms of various mental illnesses, understanding the complexities of mental health diagnoses, and learning effective communication strategies for supporting individuals in distress.
Another successful approach involves incorporating mental health awareness into existing religious education programs, using case studies, role-playing, and guest speakers to provide practical training. Finally, some faith-based organizations have developed comprehensive online resources and training modules accessible to religious leaders worldwide. These initiatives often include interactive components and opportunities for peer support.
A Structured Training Program for Religious Leaders on Mental Health
A well-structured training program should encompass several key components. The program should begin with a foundational understanding of mental health terminology, common mental health disorders, and their associated symptoms. This section would also address the crucial role of reducing stigma and promoting help-seeking behavior. Next, the training should delve into effective communication strategies, emphasizing active listening, empathy, and non-judgmental support.
Role-playing exercises would simulate real-life scenarios, allowing participants to practice these skills in a safe environment. The curriculum should also cover ethical considerations, such as confidentiality and boundaries, and the importance of referring individuals to appropriate professional services. Finally, the program should explore the integration of faith-based approaches with evidence-based mental health treatments, promoting a holistic and compassionate approach to care.
The training might include guest speakers who are mental health professionals or individuals with lived experience of mental illness. Post-training support and continuing education opportunities would reinforce learning and ensure ongoing professional development. This structured approach ensures religious leaders are adequately equipped to support their congregants effectively.
Mental Health and Religious Identity Development

Religion often plays a significant role in shaping an individual’s identity and worldview, influencing their values, beliefs, and sense of self. For many, religious practices and community involvement provide a framework for understanding life’s purpose and navigating challenges. This connection between faith and identity, however, can become complex when individuals experience mental health struggles.Religious beliefs and practices can profoundly shape an individual’s identity and self-perception.
For some, their faith provides a source of strength, comfort, and meaning, fostering a positive self-image and a strong sense of belonging. Regular participation in religious services, prayer, and community activities can reinforce a sense of purpose and connection to something larger than oneself. Conversely, rigid or overly strict interpretations of religious doctrine can lead to self-criticism, guilt, and feelings of inadequacy, particularly when struggling with mental health issues.
The internal conflict between personal experiences and religious teachings can be particularly challenging.
Religious Identity and Mental Health Struggles
Experiencing mental health challenges can significantly impact an individual’s religious identity and sense of belonging. The dissonance between experiencing symptoms like depression, anxiety, or trauma, and the expectation of unwavering faith or spiritual strength can lead to feelings of shame, isolation, and a questioning of one’s faith. Individuals may feel judged by their community or struggle to reconcile their experiences with their religious beliefs.
This can lead to a distancing from religious practices or a search for alternative spiritual frameworks that better accommodate their experiences. For example, someone struggling with depression might find their traditional religious community’s emphasis on positive thinking insufficient or even judgmental, leading them to seek support elsewhere or explore different spiritual paths.
Religious Communities Fostering Resilience and Positive Identity Development
Supportive religious communities can play a crucial role in fostering resilience and promoting positive identity development among individuals with mental health challenges. When religious leaders and community members demonstrate understanding, empathy, and acceptance, individuals feel safe to share their struggles without fear of judgment or stigma. Such environments can provide a sense of belonging, hope, and mutual support, facilitating healing and personal growth.
Examples include faith-based support groups that offer peer support and shared experiences, or religious leaders who actively promote mental health awareness and destigmatization within their congregations. The integration of mental health education into religious training programs further equips leaders to provide appropriate guidance and support to their congregants.
Interplay Between Religious Identity, Mental Health, and Personal Growth
The relationship between religious identity, mental health, and personal growth is dynamic and complex. It is not a linear progression but rather a cyclical interplay of influences.
So, where does that leave us? The relationship between mental health and religion is undeniably complex, a tapestry woven with threads of comfort, challenge, and sometimes, even conflict. While faith can be a powerful source of resilience and healing for many, it’s crucial to acknowledge the potential downsides and to approach this intersection with sensitivity and awareness. Ultimately, finding a healthy balance between spiritual life and mental well-being requires self-reflection, informed choices, and a willingness to seek support when needed – whether that support comes from a religious community, a mental health professional, or both.
Key Questions Answered
What if my religious beliefs conflict with my mental health treatment?
It’s totally valid to feel this way. Open communication with both your therapist and religious leader is key. They can work together to find a path that respects your beliefs while ensuring you receive effective treatment.
Is it okay to seek mental health help even if my religious community is skeptical?
Absolutely! Your mental health is paramount. Prioritize your well-being, even if it means navigating challenges within your community. Consider seeking support from secular resources or finding allies within your faith who understand and are supportive.
How can I find a therapist who understands my religious beliefs?
Many therapists specialize in working with diverse populations, including those with strong religious affiliations. Look for therapists who advertise cultural competence or experience working with clients of your faith background.